“Faculty of a medical school ensure that the medical curriculum provides opportunities for medical students to learn to recognize and appropriately address biases in themselves, in others, and in the health care delivery process.”
Does your institution meet that requirement?
This toolkit was formed to help explore strategies in teaching health care providers in order to reduce healthcare inequities. The discussions focus on race and racism but include a larger critical dialogue on bias, identity, intersectionality, and privilege. This toolkit provides examples of resources and activities that many are using in their attempts to teach these topics. The authors acknowledge that there are many other useful resources out there and they continue to seek them out. They hope that you will find this information useful in creating your own learning activities and that you will join them in their efforts to develop innovative, challenging and thoughtful ways to teach beyond disparities.
Dr. Larry Sherman, a Professor of Neuroscience at the Oregon Health & Science University, explains how our brains react to people who are “different” and explores possible ways to overcome the automatic prejudice that contributes to racism in our society.
Adopting an Anti-Racism Public Health Curriculum Competency: The University of Washington Experience
Seventeen-year-old unarmed Trayvon Martin was shot and killed by a Florida Stand Your Ground patrol volunteer in 2012 while walking home from a convenience store. His death launched a nationwide conversation on America’s long-sore subject of race, igniting the Black Lives Matter movement. These conversations were also held in schools and programs of public health because the field has long recognized racism as a determinant of health. But although we academics have chronicled the role of racism in shaping health outcomes, we have rarely turned our gaze inward to examine how our own schools and programs of public health perpetuate racism. Furthermore, we have largely failed to prepare our graduates with an understanding of the roots of racism and how it affects public health work.
The authors (along with others at the UWSPH) set out to develop a curriculum competency that would require all UWSPH students to acknowledge racism and its effects, to counter the tendency to minimize racism as a topic, and to compel the school to develop resources to support this education. Through this process, the authors developed a collective, although not unanimous, analysis of their role and responsibility in educating public health professionals who have the skills to name racism, address its effects, and work collaboratively with communities of color to dismantle the systems that perpetuate it. Acknowledging this responsibility is not the end, but it is an important step in a long process. In this commentary, they describe their experience in developing and adopting a new schoolwide competency, amid political pushback, and offer lessons learned to encourage other schools and programs of public health to launch their own efforts.
Interactive Modules
Exploring Racism and Health: An Intensive Interactive Session for Medical Students
Free MedEdPORTAL module
Growing recognition of the deleterious effects of racism on health has led to calls for increased education on racism for health care professionals. As part of a larger curriculum on health equity and social justice, this MedEdPortal educational session on racism for first-year medical students consists of a lecture followed by a case-based small-group discussion.
Free MedEdPORTAL module
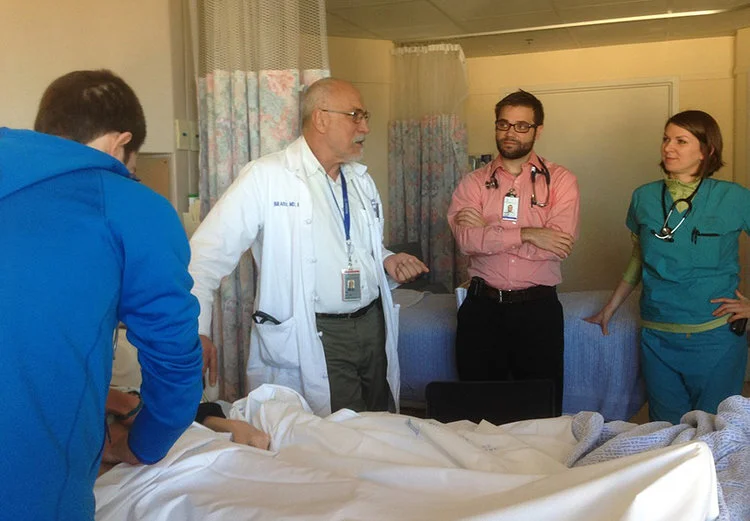
The medical community recognizes the importance of confronting structural racism and implicit bias to address health inequities. Several curricula aimed at teaching trainees about these issues are described in the literature. However, few curricula exist that engage faculty members as learners rather than teachers of these topics or target interdisciplinary audiences. This discussion of Health Equity Rounds provides a unique forum for practitioners across training levels to address structural racism and implicit bias. The aim in dissemination is to provide meaningful tools for others to adapt at their own institutions, recognizing that HER should serve as a component of larger, multifaceted efforts to decrease structural racism and implicit bias in health care.
Unconscious Bias in Medicine
This free CME activity from Stanford provides education on unconscious bias in the academic medicine workplace. Existing research on unconscious bias will provide a science-based view of this seemingly non-science topic. Case studies with examples of unconscious bias, self-assessment opportunities, and exploring bias busting strategies will enable learners to understand how to bring the content into their own unique environments.
AMA PRA Category 1 Credits™ (1.00 hours), Non-Physician Participation Credit (1.00 hours)
Free MedEdPORTAL module
There is a growing body of literature illustrating the negative impact of racial bias on clinical care. Despite the growing evidence, medical schools have been slow to make necessary curricular changes. Most attempts to educate on racial health disparities focus on transferring knowledge and do not foster the development of skills to understand one's own bias or address bias and racism in the clinical setting. To address this, we developed a small-group, case-based curriculum for rising third-year medical students. Though one session before starting clinical clerkships is not enough to maintain the practice of sustained critical thinking regarding bias and racism in clinical medicine, this session is a starting point for curriculum developers looking to use an evidence-based approach to racial bias in clinical care.
Building a Tool Kit for Medical and Dental Students: Addressing Microaggressions and Discrimination on the Wards
Free MedEdPORTAL module
Microaggressions, subtle slights related to characteristics such as race, gender, or sexual orientation, in a clinical setting can sabotage the therapeutic alliance. Curricula tailored specifically towards medical students that raise awareness of microaggressions and aim to change behavior are absent. Given the high self-reported prevalence of microaggressions in the clinical setting, students need the skills to respond. This innovative session improves readiness to address microaggressions by helping participants build and practice these skills in a supportive environment.
ERASE-ing Patient Mistreatment of Trainees: Faculty Workshop
Free MedEdPORTAL module
Mistreatment of physicians by patients is a long-standing phenomenon that has garnered increased attention recently. Medical students and residents also experience mistreatment, and many supervising physicians do not know how to recognize it or respond appropriately. Little guidance exists as to how faculty should best address these situations. The authors developed, taught, and evaluated a stepwise approach to help faculty physicians manage patient mistreatment of trainees (residents and students). The system developed fills an important void in medical education by introducing a novel, easy-to-understand approach that faculty can employ to manage mistreatment of trainees. The authors have continued to disseminate this model to faculty and residents in various departments around their medical center and at national conferences. This resource will allow educators to disseminate the ERASE model at their home institutions.